Iron and hypothyroidism
We as hypothyroid or Hashimoto’s patients have learned so much over the years about why our iron levels can fall, what labs to do, how to read those labs, why it’s NOT just about ferritin (which is simply a protein that stores iron), and how our low iron levels can push reverse T3 (RT3) up, the inactive thyroid hormone. Janie Bowthorpe, hypothyroid patient and site creator
***************************************************
7 reasons one’s iron can fall
- Being hypothyroid can result in a lowered production of stomach acid which in turn leads to the malabsorption of iron. This is probably the most common reason which covers the most people.
- Being hypo can result in heavier periods for women, which causes more iron loss on top of having low stomach acid. http://www.ncbi.nlm.nih.gov/pubmed/12754530
- Chronic inflammation can lower our serum iron levels because it pushes iron into storage, i.e into ferritin. And too many thyroid patients have inflammation. To see if you have inflammation, go here.
- Gluten sensitivity or intolerance can also cause inflammation which might lower iron.
- An allergy to what we eat can cause inflammation for some, as happened to thyroid patient Deb who discovered she was allergic to eggs. That inflammation can lower iron because it pushes iron into storage. Once she removed eggs, her iron went up!
- Gut issues, whether with Hashimoto’s or not, can lead to low iron!
- Having an active MTHFR or other methylation mutations, which usually causes a good looking or high iron, with a LOW ferritin. But that good or high iron may not be breaking down for use, putting us in a LOW IRON state. Another clue we have a methylation problem with a good looking or high iron? A TIBC getting closer to 330 or higher in the typical range, we have noticed for years now. When we are getting plenty of iron, that TIBC is usually much lower in the 300’s.
7 reasons having inadequate iron can be a problem
- Becomes the precursor to being anemic, revealed by the other iron labs—saturation and serum iron.
- Can lead to symptoms which mimic hypothyroidism—depression, achiness, easy fatigue, weakness, faster heartrate, palpitations, loss of sex drive, hair loss and/or foggy thinking, etc, causing a patient to think they are not on enough desiccated thyroid, or that desiccated thyroid is not working.
- Can make it difficult to continue raising a working desiccated thyroid with it’s 80% T4. The T4 is known to convert to RT3 in the presence of low iron.
- Can decrease deiodinase activity, i.e. it may be slowing down the conversion of T4 to T3. http://www.ncbi.nlm.nih.gov/pubmed/2498473
- May be affecting the first two of three steps of thyroid hormone synthesis by reducing the activity of the enzyme “thyroid peroxidase”, which is dependent on iron. http://www.ncbi.nlm.nih.gov/pubmed/12097675 Thyroid peroxidase brings about the chemical reactions of adding iodine to tyrosine (amino acid), which then produces T4 and T3. Insufficient iron levels alter and reduces the conversion of T4 to T3, besides binding T3. Additionally, low iron levels can increase circulating concentrations of TSH (thyroid stimulating hormone).
- Can negatively effect the production of cortisol via the adrenal cortex. This study reveals that an iron-containing protein is present in high amounts in the adrenal cortex and is involved in the synthesis of corticosterone. So by having low iron, you can potentially lower your cortisol levels.
- Can have a negative effect on your body’s ability to produce/break down for use thyroid hormones (in addition to iodine, selenium and zinc) http://www.biomedcentral.com/1472-6823/8/2
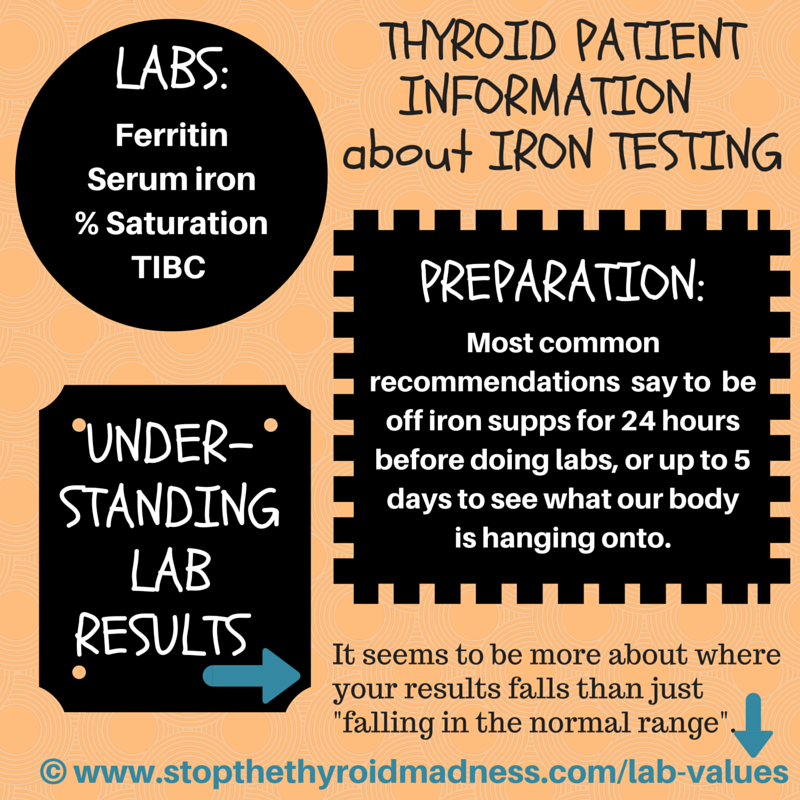
What iron labs we need: where we should fall in ranges
It’s about four labs: serum iron, % saturation, TIBC (or IBC), and ferritin.
For iron in US ranges, women generally fall around 110. Their % saturation generally falls at 34 or 35%. Their ferritin generally falls starting in the 50s, but can go up to the 70’s. NOTE: ferritin is not iron. It’s a protein that stores iron. We DO NOT treat ferritin. The latter is just information. Instead, we look at ferritin to see if we have inflammation. The body will push iron into this storage if we do have inflammation.
For men, their iron in US ranges, they generally fall in the upper 130’s. Their % is around 38, give or take. Their ferritin is around 110.
In summary: it’s four iron labs we learned that we need: serum iron, % saturation, TIBC and Ferritin…NOT just ferritin, which is NOT iron. It’s a storage protein. We stay off iron for 24 hours, or even better, 5 days to see what we are hanging onto. To see where patients fall when iron is optimal, this page will help-it’s based on years and year of observations: www.stopthethyroidmadness.com/lab-values
Can I only measure ferritin, aka a protein which stores iron, and/or treat based on ferritin alone?
Big mistake, we have learned repeatedly over the years!
Yes, low ferritin can go hand-in-hand with low iron. But low ferritin can also occur with high iron due to stress!! Several of us have experienced this reason for high iron with low ferritin! And it means we are in a low iron state. And common to this scenario, our TIBC will be too high, i.e. not in the bottom 300’s where is should be with healthy iron (of a range similar to 250-450)
Less common is having an active MTHFR mutation which can push heavy metals high.
So by treating that low ferritin alone, we can push our iron and % saturation levels even higher! Not a good thing.
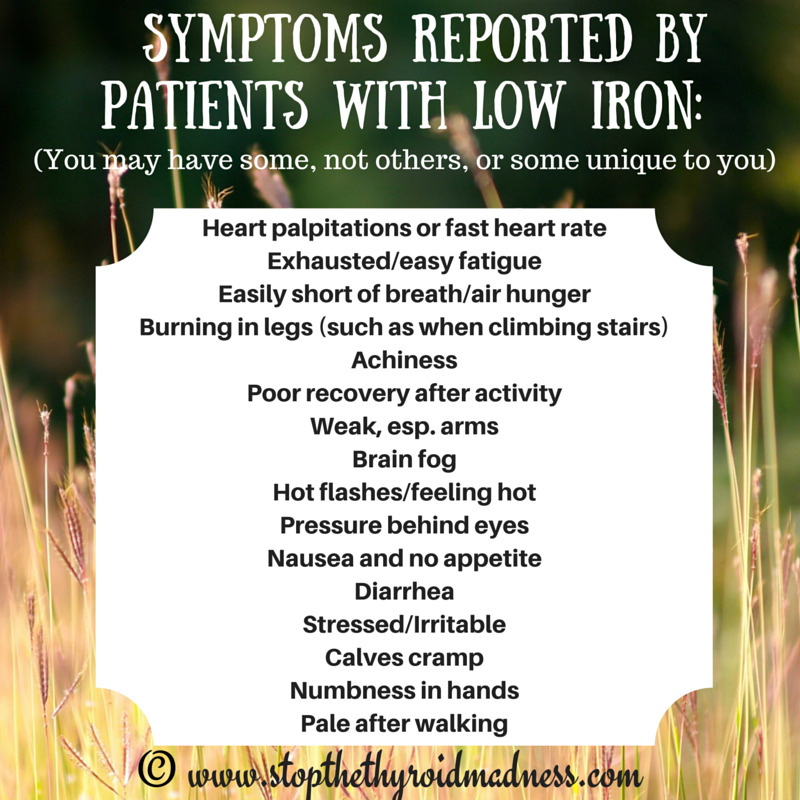
POTENTIAL SYMPTOMS OF HAVING LOW IRON
Summary: symptoms of having low iron include heart palps or fast heartrate, easy fatigue (similar to hypothyroid), short of breath or air hunger, burning in legs when climbing stairs due to increased lactic acid, achiness, poor recovery after exercise, weakness, brain fog, hot flashes or feeing hot, pressure behind eyes, diarrhea, stressed, irritable, cramps, numbness, pale after walking, etc.
Summary on how to get iron, supplementation, amounts and more we’ve learned as patients
a) High iron foods in one’s diet
Now granted, this won’t be as effective as being on supplementation. But if serum iron is only low in a minor way (see the Lab Values page to know), it might work, report patients. Foods rich in iron include lean meats, liver, eggs, green leafy vegetables (spinach, collard greens, kale), wheat germ, whole grain breads and cereals (though not for those with gluten problems), raisins, and molasses. Some cook their foods in a cast iron skillet. Remember that to be effective, we as patients discovered we need an acidic environment in our stomach to properly absorb the iron. If in doubt, we make sure to put lemon juice or ACV (apple cider vinegar) in water and drink while eating iron rich foods.
b) Supplementation
This has been the most effective if iron is low. There are all sorts of iron products out there! One favorite is Iron Bisglycinate because it seems to cause less constipation, plus the milligrams on the bottle equal the amount of elemental iron in the tablets, whereas the other may not. See below on how much. There are whole food versions of iron which can be made from beet root or liver, but two cautions: they can take longer, and liver also has high amounts of copper.
From Canada, there is a chewable non-constipating iron called Hemofactors by Natural Factors, and one patient who wrote me swears by it. It’s Ferric Pyrophosphate, also called SunActive Iron and you’ll want to pay attention to the “elemental iron” amount to get enough. Here’s one that patients are reporting takes only two tabs a day to raise iron: Proferrin ES Heme Iron Polypeptide It’s from bovine sources. But we need more experiences to know for sure if only two will do the job for all….and it may have high copper.
Beware of “liquid” iron that is animal based (heme)—it may be the best absorbable iron, but it can blacken your teeth, as it did to the owner of this site. One suggested solution is to use a straw when taking the liquid iron. VEGETABLE BASED (nonheme) liquid iron avoids this, even if less absorbable. Also, because liquid heme iron is much more absorbable, patients take far less to achieve the same results as tablets.
c) How much iron supplement to raise low iron levels, and how long do patients report taking it?
For most of the above (except the bovine source), it’s NOT about taking one or two tablets, a mistake many patients say they made. The body uses it up.
Patients have discovered they usually need 150 to 200 mg of “elemental iron” daily, spread out with meals (i.e. 3 times a day), in order to adequately raise their iron levels. Always check your labels or call the company to see how much “elemental iron” is in each tablet. We’ve noticed it can take a minimum of 6-8 weeks to improve our levels to the desirable goal. Patients keep track of lab work to see where levels are. Some women who are menstruating may have to stay on maintenance amounts of iron.
Liquid is far more absorbable, so we may not need as much “elemental iron” as tablets. But it’s hard to know how much will raise your iron. Labs will help. Beware of liquid heme iron–it can blacken your teeth.
Please work with your doctor on this.
d) Another way of using supplementation!
An interesting new way was reported by Dr. Allen Green about research showing to take iron every other day! BUT…we don’t have much experiences on this, and it seems you’d have to take the 150 – 200 mg every other day to make it work…if it works.
WARNING: literature states that if you have cancer, taking iron can promote cancer growth. Talk to your doctor before deciding this information is right for you.
e) What we learned to take with iron for better absorption?
Yes, say patients, two things: an acid in the drink (lemon juice or apple cider vinegar, such as one tablespoon or more) and Vitamin C in supplement form to tolerance each time, or high Vitamin C foods. That vitamin C improves iron absorption and our experiences have proven it. I Janie, tolerate 3000 mg VItamin C each time I take iron because I’ve been on C awhile. You may have to start lower to prevent diarrhea and just slowly build up.
Also taking a mineral supplement can assist the absorption, as can B12. One important B-vitamin is Folate (not Folic acid), which promotes red blood cell formation. Adding it to your iron supplementation can be key, some patients have reported. But if you have MTHFR, be careful going too high — it helps increase the breakdown and release of toxins or metals, and you have symptoms of that, or excess fatigue. Moderation.
f) What we as patients learned to avoid in our stomachs when taking iron
Literature says to avoid calcium, coffee, tea or wine (tannins are said to interfere with absorption to some degree), the fiber of bran, and chocolate at the same time we take iron. Patients report also avoiding a mix of iron with thyroid pills, and separating the two, whether one hour, two hours, or four hours. It varies and we guess it may depend on one’s metabolism in digesting the iron.
Do we as patients take iron at the same time we take thyroid meds like NDT or T4/T3 or T3?
Patients report avoiding swallowing iron at the same time as thyroid pills, since the iron will bind to some of the thyroid hormones as they mix in your stomach and bind some thyroid hormones. They might take their T3 or desiccated thyroid one hour before iron is taken, or several hours later…or try their best to keep them apart somehow. (If you are doing your natural thyroid sublingually, some may end up still being swallowed and thus mixed with that iron, but we’re not sure how much of a problem that is…. So just use your best judgment.)
What are problems patients have reported when taking iron
Constipation is common–here are solutions
Patients report adding Magnesium Citrate or other kinds of magnesium as a supplement, taken twice a day, until they find the amount that softens their stool. They know within a few days if the amount being taken is enough….or even too much (i.e. too much will cause diarrhea). But iron bisglycinate usually avoids the constipation.
Why do some feel they aren’t tolerating iron supplements
For one, low stomach acid can cause problems, causing iron to sit in the stomach too long. So these patients drink it down with an acid in the drink, like lemon juice or ACV mixed with water or other liquid. Some report they start on less than others, then slowly built up. Or if there are problems absorbing oral iron due to a previous stomach surgery or other issues, another option is to use Venofer — an intravenous iron which helps replenish body iron stores. Talk to your doctor about this, though. See below.
What about iron injections or IV?
If iron labs are seriously low, some doctor prescribe an iron injection or prescribing an IV iron infusion. Either will raise your iron levels far quicker just a few weeks as compared to a several weeks from supplementation. The IV infusion does require being in a health facility and it can be expensive. You will be monitored to prevent anaphylactic shock. Patients will often follow that up in a few weeks by staying in lower doses of oral iron tablets.
What we learned to do during supplementation, and after..
During supplementation, we found out the hard way to test our iron again in about 4-6 weeks. We don’t want to overload ourselves with iron, and some patients have had that happen when doctors make them wait too long! Or we could have hemochromatosis and not know it! Also, you could have what’s called the MTHFR genetic defect, which means your body doesn’t do a good job breaking metals down. Thus, your iron could get too high. ALWAYS retest, we have learned!
Once I get my iron levels up, does it stay up?
For females, some of us have had our iron levels plummet again, so it may be wise to stick with a small dose of supplemental iron or eat iron rich foods, especially if you are female and still menstruating. Once into menopause, your iron levels may stay where they need to…but they may not! Work with your doctor.
MISCELLANEOUS TOPICS
Do patients report being able to to raise iron without being on iron supps?
Possibly…if someone isn’t severely anemic, and are just not totally optimal! One thyroid patient reports that just by getting on NDT and finding her optimal amount, she saw her iron levels go to an optimal level. Others focused on consuming high iron foods. You can see where optimal iron results should be, here.
Are men different than women in their iron lab results?
Yes. Men normally have higher levels of iron than women, such as the 130’s in US-type ranges, we’re noticed on labs. Additionally, it’s common to see healthy men with a ferritin slightly over 100, like 110-ish. See the lab values page.
QUESTIONS PERTAINING TO IRON LAB RESULTS:
My TIBC is low as is my iron. What does that mean for me? TIBC stands for Total Iron Binding Capacity, and it’s basically telling you how much protein your liver is making in order to envelope and carry that iron around. Typically, if iron is low and you make enough of this protein called transferrin, TIBC will be higher in the range, such as nearly 350 is US ranges (US ranges are generally 250-450, so if you live in a country with a different range, you can figure it out based on that). So if your TIBC is low, it might mean three things, say literature 1) Your liver needs support! Milk Thistle and Dandelion Root are two supportive supplements. 2) You can’t take the high amounts of iron that others do with low TIBC, since it will be problematic without that protein 3) You’ll need to consider taking lactoferrin with each dose of iron to supply the needed carrying iron. Because of lactoferrin, you might be able to take the higher amounts.
What if I find that THREE of my iron results are high…aka Ferritin, Serum iron and % Saturation? This is called an iron overload, such as the inherited disorder called hemochromatosis. Testing is needed, though, to confirm it. Then your doctor will usually direct you to give blood in order to lower these harmful higher levels. With hemochromatosis, you can have a low TIBC or UIBC. (NOTE: Another cause of high levels of iron is having a defect in the MTHFR gene or any other methylation issue, meaning the body isn’t breaking down iron for use, but it will usually mean low ferritin, unlike hemochromatosis).
What causes low ferritin when other labs look great or are even too high? That usually points to an MTHFR mutation and having high heavy metals. You can also see high levels of homocysteine with this defect, as well as higher levels of copper and other metals.
DIDN’T DO YOUR PERCENT SATURATION LAB?? If you did both TIBC and Serum iron, you can figure out your percent saturation right here.
*******************
MISCELLANEOUS:
— Need a good doctor to work with in all this? Go here. Remember this is all about information and shouldn’t replace that relationship.
— Get your own iron labs ordered and done via the Recommended Labwork page
— AS FAR AS THE 70-90 RANGE FOR FERRITIN: there were five scholarly articles on the net referring to this 70-90 range from 2004 to 2012…but they have all disappeared i.e. the websites disappeared from the net. So most of what you will see on the internet are websites which saw this range on Stop the Thyroid Madness (and fail to give STTM credit—sadly common), and we at least had studies or articles to prove it. Now we don’t.
ADDITIONAL READING
– Taking iron every other day: https://www.drgreene.com/decreasing-iron-supplements/
— Details on iron: http://www.fao.org/DOCREP/004/Y2809E/y2809e0j.htm
— How low iron affects cortisol: http://www.ncbi.nlm.nih.gov/pubmed/1651678
— Impaired conversion of T4 to T3: http://ajpregu.physiology.org/content/239/5/R377
— Low iron and sympathetic system: http://www.ncbi.nlm.nih.gov/pubmed/17660705
— Iron and selenium deficiencies on iodine and thyroid metabolism found here.
— Iron Deficiency in Goitrous Children article found here.
— Iron Supplementation for Unexplained Fatigue in Non-Anaemic Women article found here.
— A good article explaining supplements to take with iron found here.
JOIN THE STTM FACEBOOK PAGE for daily inspiration, tips and fellowship with others!!
Important note: STTM is an information-only site based on what many patients worldwide have reported in their treatment and wisdom over the years. This is not to be taken as personal medical advice, nor to replace a relationship with your doctor. By reading this information-only website, you take full responsibility for what you choose to do with this website's information or outcomes. See the Disclaimer and Terms of Use.